We think that, wealth of a nation means the GDP growth rate , national infrastructure development, less fiscal deficit, welfare schemes of the government. Yes it is, but it also includes Good Health Infrastructure(HI). To build a healthy nation, spending on (HI) has most significance because,“ Health is wealth”
Countries with high HDI like Sweden, Norway provide free health care services to their citizens. In India, we cannot expect to become like developed countries because there are certain problems associated with the health sector.
What are the problems?
Low Expenditure on Health
The combined expenditure of Centre and States on health is around 1.5% of India’s GDP. It is much below the target of 2.5% as proposed in the National Health Policy, 20171.
Higher Out-of-pocket Expenditure on Health
The out-of-pocket expenditure as percentage of total healthcare expenditure is as high as 60% on account of expenses incurred on medicines, diagnostic tests, consultation fees2.
Lack of Affordability
The contribution of the private sector in healthcare expenditure in India is around 80 % while the rest 20 % is contributed by the Public Sector. The private sector also provides for 58 of the hospitals and 81% of the doctors in India3. However, since the private sector hospitals work on the profit motive and charge high fees, the Private sector hospitals do not address the needs of the poor patients.
Lack of Accessibility:
Most of the secondary and tertiary care hospitals are located in Tier-1 and Tier-2 cities. Similarly, most of the doctors are unwilling to practice in rural areas.
Changes in Demography
India is set to undergo demographic transactions in the next two decades where the share of elderly population is said to increase from 8% (2011) to 16% (2041). The change in demography accompanied by increase in the lifestyle diseases would put additional burden on the existing health care infrastructure4.
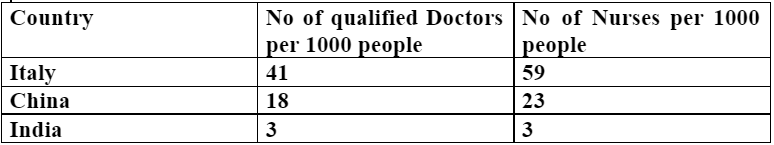
Lack of Medical Personnel
The statistics show the need for increased public spending on health infrastructure .Italy is a less populated country with 6 crores population, yet they give priority to the health sector6. India has a vast population of 139 crores. So the need to focus on health infrastructure is significant.
Recently we have witnessed Covid-19 pandemic across the world. Even developed nations like the US, Italy were unable to overcome the Covid- 19 crisis.
So, what about India?
The second Tsunami wave (Covid 19) is severely affecting the people of India.The main reason is poor health infrastructure.
1. Lack of sufficient beds in the hospital
2.Shortage of oxygen cylinders.
3.Less number of government hospitals
4. Poor functioning of primary healthcare centres .
5.Higher treatment charge in Private hospitals.
Recently in Kerala, the tribal people in the Palghat district have started to make a pocket road in the forest area to reach the primary healthcare centre, which is 14 kms away. For many months they were protesting against the decision of the environmental department to not build a road citing environmental concerns7.
In Odisha, a man walked kilometers carrying his wife’s dead body because of lack of proper medical facilities.
We all witnessed the covid patient’s pathetic situation in Delhi and various parts of the country because of lack of oxygen supply. So, the health sector should be considered as a priority sector and we should make proper planning to improve it.
RECOMMENDATIONS:
The 15th Finance Commission has mooted a greater role for public private partnerships to ramp up health infrastructure and scale up public spending on health to 2.5% of GDP by 20248.
The Public-Private-Partnership (PPP) in the field of healthcare is a form of agreement between the Government and Private sector for providing various healthcare services to the people. It seeks to leverage the private sector’s strength of innovation and efficiency. Further, it redefines the role of the government from being a health service provider to being both provider and financer of healthcare services. It may take different forms depending upon the extent of participation of the private sector. (Finance commission)
Example: It may involve contracting out the management of Primary Health Centre at village level to the private sector. It may be in the form of Government providing Healthcare Insurance on secondary and tertiary treatment in the private hospitals (PM Jan Arogya Abhiyaan).
What are the possibilities?
Effective and Affordable Medicines:
The government is presently implementing the Pradhan Mantri Bhartiya Janaushadhi Pariyojana (PMBJP) in order to provide cheaper generic medicines through the network of Janaushadhi Kendras. Now,this is a kind of PPP Mode for mainly two reasons.
Firstly, it involves procurement of bulk generic medicines from the Private sector. Secondly, it enables the non-governmental entities such as NGOs, Private Sector hospitals etc. to set up Janaushadhi Kendras9.
Improvisation of Preventive Care: The Civil society organisations (CSOs) can contribute effectively to community mobilisation, information dissemination, community-based monitoring of health services and capacity building of community-based organisations and workers. Hence, the CSOs can be leveraged under PPP mode to improve the health outcomes of the government schemes such as National Health Mission (NHM).
In Kerala , there is healthy collaborative working between the Local Self Governments and Primary Healthcare Centres,the workers of Integrated Child Development Scheme(ICDS) like Asha workers provide proper information about the healthcare schemes to the people in their ward. These workers are also called RAPID RESPONSE TEAM. This system should be implemented in every state in India.
Public-private partnerships and collaborations, for instance, the Defence Research and Development Organisation (DRDO) has developed ventilators, collaborated with industry to scale up production of ventilators.
Recently DRDO ( Nuclear medicine and allied science ) developed medicine Called (2-DG ) for the second tsunami wave , this shows that collaboration in the field of healthcare is a good initiative.
The government has made several interventions in the health sector including National Medical Commission, National Digital Health Mission, Ayushman Bharat, etc. National Institute of Health and Family Welfare (NIHFW), has implemented the “Public Health Systems Capacity Building in India” project. 17 Global Health Security Agenda (GHSA) projects have been started in India, with different government and private organisations10.
Proper implementation of the present government healthcare schemes will improve the health infrastructure of the country .But there are certain challenges.
WHAT ARE THEY?
1. Lack of proper Implementation
2. Unawareness among people
3. Improper Administration
4. Sale of medicines to private medical shops
5. Link between the doctors and medical representatives
Recently, the World Health Organization (WHO) in a report held that vaccine hesitancy is among the top 10 threats to global health in 2019.
Vaccine hesitancy has been reported in more than 90% of countries in the world. WHO defines vaccine hesitancy as a delay in acceptance or refusal of vaccines despite the availability of vaccination services11.
Global Health Security Agenda (GHSA), set in 2014, builds on the WHO International Health Regulations (IHR) that provide guidance for countries12 to assess and manage serious health threats that have the potential to spread beyond borders.
Thus, we have a number of government initiatives to make healthy Healthcare Infrastructure. Proper planning and implementation is needed for a good Healthcare Infrastructure in the country.
"The views and opinions expressed in this article are those of the author and do not necessarily represent the views of The Renaissance"
Ministry of Health and family welfare. National Health policy 2017. ministry of health and family welfare, 2017 ↩
Ministry of Health and family welfare. National Health policy 2017. ministry of health and family welfare, 2017 ↩
Finance Commission. Finance Commission on Covid times Report. Finance Commission, 2020 ↩
Finance commission. Finance Commission in Covid Times Report for 2021-26. ↩
Finance commission. Finance Commission in Covid Times Report for 2021-26. ↩
Raus Current affairs. health. Raus, 2021 ↩
Tribal Associations. Need for primary Healthcare services. ↩
Finance commission. Finance Commission in Covid Times Report for 2021-26. ↩
Ministry of Health and Family welfare. various projects. MOH, 2020. ↩
Poornalingam. “Building a robust Healthcare system.” The Hindu, 1 February 2021. ↩
World Health Organization. WHO Health Report. WHO, 2020 ↩
WHO. WHO International Health Regulations. WHO, 2014. ↩



